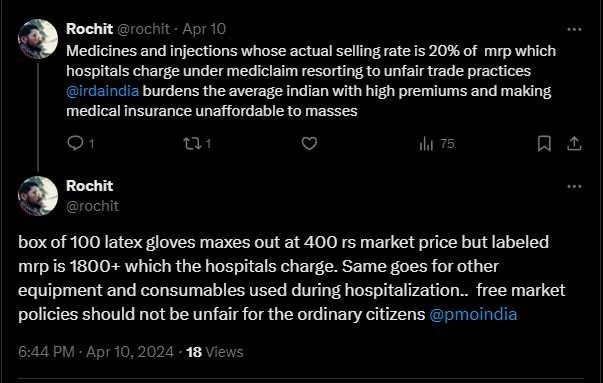
Will Standardized Medical Costs Improve Healthcare in India?
By Arunima Rajan
The Supreme Court's active role in attempting to regulate healthcare costs signifies a pivotal moment for India's healthcare policy, sparking discussions on justice, accessibility, and affordability in healthcare. Arunima Rajan explores the need for a fair, standardised pricing mechanism in healthcare to ensure affordability and accessibility.
The Supreme Court of India, in response to a public interest litigation (PIL) filed by an NGO, Veterans Forum for Transparency in Public Life, has issued a landmark directive. This directive, which mandates the Union government to establish standardised rates for various medical procedures across the country, is a significant step towards ensuring equitable healthcare. The court's decision was prompted by a stark contrast in the charges for medical treatments between government and private hospitals, a disparity it deemed unacceptable.
Highlights Broader Issue of Healthcare Inequality
The Supreme Court has given the Union Health Secretary a deadline to work with state and union territory governments to develop a proposal for standardised hospital charges within a month. If the government fails to comply, the court may consider implementing rates applicable to Central Government Health Services (CGHS)-empanelled hospitals as an interim measure. This directive aims to ensure citizens have access to affordable healthcare, a fundamental right.
Clinical Establishment Act and its Implementation Challenges
The Central Government has enacted the Clinical Establishments (Registration and Regulation) Act to regulate all clinical establishments in the country and prescribe the minimum standards of facilities and services they provide.
Rule 9 of the Clinical Establishment Act Rules of 2012 states that
(i) Every establishment shall display the rates charged for each type of service provided and facilities available for the benefit of patients at a conspicuous place in the local and English languages.
(ii) The establishment shall charge the rates for each type of procedure & service within the range of rates determined & issued by the central government from time to time in consultation with the state government. "While complying with clause (i) is not an issue as most hospitals in general and NABH accredited hospitals do maintain & publish rates. The main issue vide clause (ii) is about fixing rates. No study has been conducted to determine medical procedure costs," says Girdhar Gyani, Director General of the Association of Healthcare Providers India (AHPI).
Laissez Faire cannot be allowed in the Health Sector
"This is an important issue, and regulated pricing should have been implemented years ago. Every service has a fixed range of pricing appropriate authorities determine, whether airlines, railways, insurance, education, etc. Why should health services be an exception? Since healthcare often deals with life and death situations, it needs even more stringent regulatory and price control. For example, historically, when drug prices were controlled in India, pharma companies were still highly profitable. Regulations must be comprehensive regarding what service is provided and at what cost. Health services are prone to supply-induced demand, with providers determining what needs to be done, and often, these decisions about procedures, diagnostics, and surgery may be irrational and unnecessary and, hence, a tendency to inflate costs. The price of each service component must be cost-based. Insurance companies fix rates for different procedures, so why can't governments? The price of a Stent or a diagnostic test cannot be vastly different across hospitals. There has to be some sense, logic and ethics. Price regulation is necessary if we want affordable care and the private sector to survive. Laissez-faire cannot be allowed in the health sector. Healthcare is not a commodity but a humane service. Private health providers must realise this in the interest of their patients for their survival," says Ravi Duggal, a public health activist.
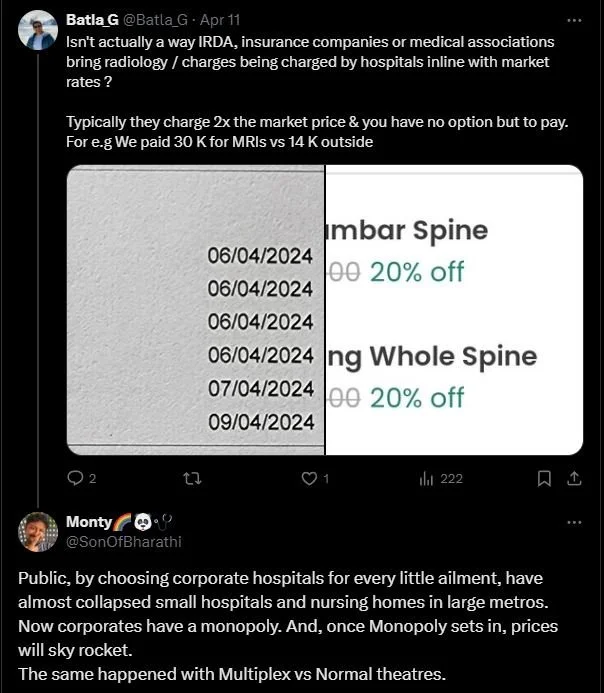
The Supreme Court's directive has understandably raised concerns among private healthcare institutions. They argue that standardising rates could harm their operations and the quality of healthcare services they provide.
Feasibility of Implementing Uniform Pricing
There are numerous challenges to implementing uniform prices across private hospitals in the country. "Costing of medical procedures is indeed very complex. The cost will vary based on the hospital category, such as primary, secondary, tertiary, or quaternity care. Capital and operational cost variation will also depend on location in Tier-I/II/III or rural settings. Then, there is variation in cost depending upon the application of technology, such as performing surgery through open, laparoscopic, robotics, etc. All this needs to work based upon activity-based costing, which can be done by authorised bodies like the Institute of Cost Accountants of India," explains Gyani.
"CGHS rates are not arrived at based on any scientific study. These were derived from inviting quotations from hospitals/ nursing homes; the lowest was fixed as CGHS rates. Further, these rates were fixed in 2014 and have not been revised. Most of these rates do not cover the operational cost of hospital procedures. To meet the obligation to serve government beneficiaries, hospitals provide services to beneficiaries at CGHS rates, which is not more than 30% of the patient load. Patients come through CASH or private insurance, which provides cross subsidiary. Applying these rates for 100% patients will be detrimental to the very sustainability of healthcare establishments," explains Gyani.
AHPI has written to the government, bringing out all relevant facts and explaining that it will not be feasible for hospitals in general and tertiary care, mainly, to work at CGHS rates. "AHPI has also filed an intervention in the Hon Supreme Court, and hopefully, our stand will be sympathetically heard by the Hon Court," explains Gyani.
Financial Sustainability
The healthcare business is largely equity-based. The Hon. Supreme Court issued the directive, which negatively impacted stocks. Some financial institutions invited AHPI to interact with their members to ease the fear. Luckily, stocks have recovered, but an element of uncertainty remains.
Only a few states have implemented the Clinical Establishment Act. What are the practical challenges in implementing it?
"Implementing regulation directly by the government is always a challenge. Globally, the government relies on third-party agencies to implement regulations. Good examples are IRDAI, TRAI, and FSSAI in our country. We have suggested that the government appoint an independent Regulatory Body for Hospitals, which can work objectively on all issues," explains Gyani.
"Universal Healthcare Coverage is defined as providing healthcare at a cost the population can afford. The government has PMJAY, which allows 40% of the underprivileged population to get free healthcare of INR 5 lakh. To avail of tertiary care, the beneficiary under this scheme has to turn to private hospitals invariably. Once again, the reimbursement rates under PMJAY are abnormally low and unviable. The government should revise the rates or allow hospitals to charge co-payments for certain high procedures. The government may also include senior citizens over 65 in the PMJAY. The rest of the population should be encouraged to take private insurance coverage," adds Gyani.
Tricky Issue
"Standardisation of the pricing of Hospital services is a tricky issue. We cannot easily ascertain the Price of Hospital services like an FMCG product, where the fixed and variable costs can be easily understood. Activity-based costing allows for determining prices for common procedures without complications, such as cataract surgery and hernia repair. Also, the quality of Physical infrastructure, availability and quality of workforce and consumables varies from hospital to hospital. Like the Maximum Retail Price ( MRP ) for an FMCG item, there needs to be a thought on the concept of Maximum Service Price ( MSP ) for hospital services, particularly procedures that can be done after a careful study by Hospital groups, civil society groups and the government. If you take OPD services, you will find huge variations across hospitals and cities. For example, hospital OPD charges in Mumbai are much higher than in Hyderabad or Thiruvananthapuram. The major obstacle in standardising the prices is the complexity and complications in critical areas Like ICU, OT services, etc. In the initial stage, rates can be fixed (Maximum service price ) for laboratory and radiological services. This also comes with a condition." For example, some of the hospitals may be using refurbished equipment, which may compromise patient safety and can get the standardised charge when compared with a healthcare provider who uses the latest state-of-the-art technology in diagnostics," says Feroz Ikbal, Associate Professor at Tata Institute of Social Sciences.
Sandy Khanda, a public health advocate, seconds his views. "Implementing standardised medical costs can be challenging due to various factors: 1. Complexity of Healthcare Systems- Healthcare systems vary widely across regions and countries, making it difficult to establish uniform standards that accommodate these differences. 2. Resistance from Stakeholders- Healthcare providers, insurance companies, and other stakeholders may resist standardisation efforts if they perceive it as a threat to their autonomy or financial interests.3. Technological
Integration- Integrating standardised medical costs with existing healthcare IT systems can be challenging and expensive..4. Public Perception and Acceptance- Patients and the public may have concerns about how standardised costs could impact the quality and accessibility of healthcare services," he explains.
Saurab Jain, co-founder and chief business officer of Eazymed Technologies Private Limited, has a different take on the issue. "Standardising medical costs can go two ways. If the standard pricing is set to be high, like in the case of private hospitals, then the government will shell out more than it does today. But, if it becomes the other way around, where the costs are standardised based on government pricing, the private players will be affected. I would say that the medication cost be standardised across the board so that the patients, regardless of socio-economic status, pay the same price. It will enable many patients to access speciality medicines, which usually cost anywhere between INR 10,000 to INR 2 lakh per month," he concludes.